9 Scientifically Backed Reasons To Eliminate Gluten

Gluten is a topic that can divide friends, cause arguments, and disrupt quite a number of dinner parties. So before we dive into any lists, let’s get some information on the table.
Many people have adopted a gluten-free diet to combat modern digestive diseases such as irritable bowel syndrome, Crohn’s, and ulcerative colitis. However, gluten is most well-known for its role in the development of celiac disease, an autoimmune condition affecting the integrity of the intestinal cells in genetically predisposed people.
Even some chronic disorders that aren’t normally associated with digestive distress like schizophrenia, attention deficit hyperactivity disorder (ADHD), multiple sclerosis, Parkinson’s, Hashimoto’s, and Alzheimer’s disease may be aggravated by the body’s attempt to deal with this complex grain protein.
While most people understand gluten’s association with wheat, most are unaware of its chemical makeup and its implications for human health, even in individuals who aren’t genetically susceptible to developing celiac disease.
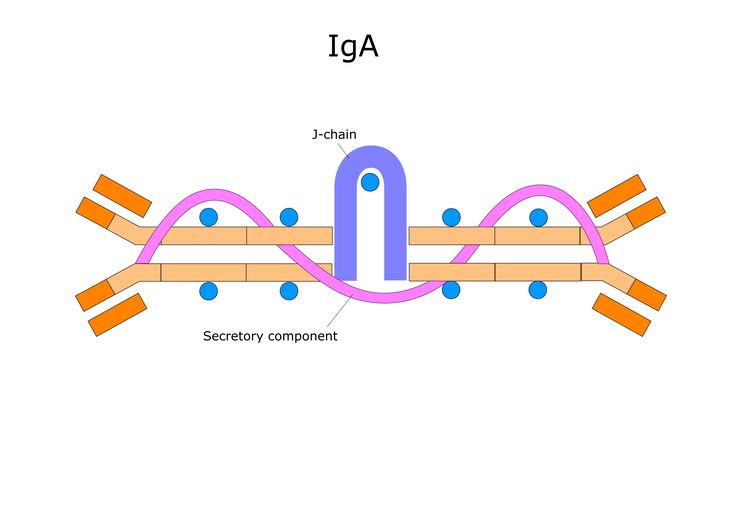
A true wheat allergy, when the immune system creates life-threatening IgE antibodies in response to wheat exposure, is acknowledged by most health authorities. However, the idea that people can have a chronic inflammatory response to undigested wheat gluten is mostly denied by conventional health institutions.

Gluten Translates to “Glue”
Gluten is a collective term for a matrix of proteins found in some grains, including wheat, barley, rye, triticale, spelt, and kamut. Since wheat is the most commonly consumed gluten-containing grain, we’ll focus on wheat gluten specifically.
The main components of gluten are the glutenins and gliadins, two distinct types of proteins that interact when hydrated to form a sticky protein matrix bonded by strong disulfide bridges. The network of peptide strands captures carbon dioxide created by the yeast in the bread, and all this comes together into a gluey mix. Gluten can also be found in many processed foods and cosmetics that aren’t commonly associated with wheat.
But glue isn’t food, which is something we learned early in our childhood. Although the formation of this wheat “glue” is convenient in making light, fluffy baked goods, chewy doughs, thick creams, and gels, it’s quite hard for your body to take apart and assimilate.
It’s impossible to break down the gooey mess into its amino acid building blocks, leading to the absorption of larger protein aggregates that initiate an inflammatory response, particularly to the gliadin peptides (protein chain) once they’re found circulating in the blood stream. Since inflammation has been linked to several chronic diseases, it’s clear how gluten sensitivity may also contribute to their development.
The Gluten Sensitivity Spectrum
Our inability to completely digest gluten has resulted in an immune response to residual gluten in the gastrointestinal (GI) tract. Sensitivity to gluten can be broken up into three categories:
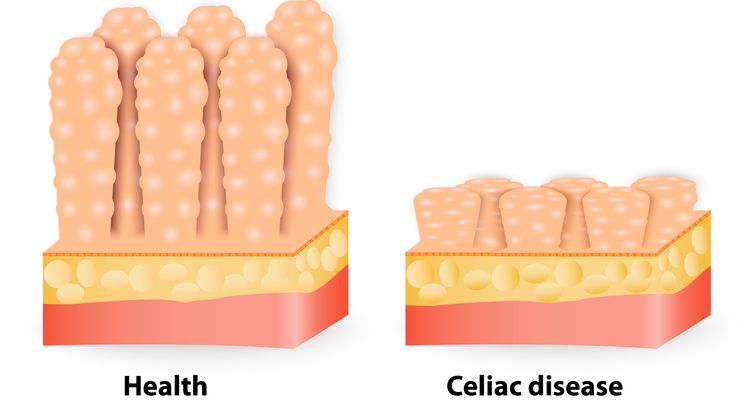
1. Celiac disease (CD) is an autoimmune disease triggered and perpetuated by intake of gluten. It’s the most extreme case of gluten sensitivity. In this disorder, the immune system makes antibodies for gliadins, but it also makes them against transglutaminase, an enzyme produced by the cells lining the intestines.
The attacks on transglutaminase over time degrade the microvilli, the tiny hair-like extensions of intestinal cells that enable maximum nutrient absorption. This blunting of the microvilli, accompanied by severe digestive distress with exposure to gluten is characteristic of celiac disease. However, other manifestations of celiac disease may include ataxia (coordination issues) and dermatitis (skin rashes).
2. Non-celiac gluten sensitivity (NCGS) isn’t an autoimmune condition triggered by gluten; rather, it’s a low-level inflammatory response to one or more of gluten’s components that can affect nearly every system in the body, including your gut, internal organs, and even your brain, depending on genetic predisposition. Since the effects of NCGS are different for different people, it’s difficult to diagnose gluten sensitivity, making it a controversial diagnosis from the perspective of most conventional medical institutions.
3. At the opposite end of the spectrum is the third category—people who are tolerant of gluten. That is, they don’t have any adverse effects when they eat gluten and don’t have measurable gliadin antibodies.
Regardless of where you fall on the above spectrum, there are many reasons why you ought to avoid gluten altogether. The following list will almost certainly make you consider taking immediate action.

1. It’s Impossible for Anyone to Fully Digest Gluten
Even if you’re tolerant of gluten-containing products, Dr. Tom O’Bryan, DC, an expert in gluten, points out that our bodies aren’t equipped with enzymes to break down gluten or its constituents, particularly the gliadin peptides. O’Bryan also emphasizes the findings of Alessio Fasano, a gastroenterologist and researcher from Harvard Medical School who has dedicated much of his research to gut permeability and the development of celiac disease.
Fasano observed that gluten doesn’t dissolve in a solution of concentrated hydrochloric acid. Since this is the acid in our stomach that’s responsible for digesting our food, it would follow that gluten digestion is at a disadvantage early in the digestive process, particularly in people who already have low stomach acid.
Amy Myers, MD, a specialist in the treatment of autoimmune disease, also points out that there are chemicals naturally produced by grains that reduce the secretion of digestive enzymes. One study examined that wheat was effective at inhibiting both α-amylase from human saliva and trypsin from porcine pancreas.1
These observations taken together explain why most of the gluten we digest ends up only partially digested and may contribute to a decrease in total digestive capacity.
2. Undigested Gluten = A Feast for Bacteria and Yeast
Myers also points out that as a result of our inability to break down gluten, the partially digested matrix of proteins ends up sticking around in the digestive tract, allowing fermentation by bacteria and yeast.
This in turn can lead to gut dysbiosis, characterized by an imbalance of good and bad bacteria. It could also cause the development of small intestinal bacterial overgrowth (SIBO).2 Gut dysbiosis contributes to chronic inflammation by increasing the load of pro-inflammatory cytokines.3
The resulting imbalance and improper location of bacteria in the GI tract have also been linked to autoimmune diseases by contributing to intestinal permeability, also known as “leaky gut.” Fasano found that pathogenic bacteria in the small intestine (SIBO) also upregulate the release of zonulin, a molecule that opens the tight junctions between intestinal cells, contributing to the development of a leaky gut.4
When the gut becomes leaky, undigested proteins, including undigested gluten aggregates, are able to escape into the bloodstream and potentially cause an inflammatory response. Over time, this may contribute to autoimmunity.
3. Gliadin Causes Leaky Gut
Fasano also found that it’s not just bacteria in the wrong place that contributes to upregulated zonulin—the gliadin component of gluten itself can do this too, regardless of whether or not a person has celiac disease (CD). The only thing that differs between people with CD, NCGS, and gluten tolerance is what happens after the gate between intestinal cells is opened by zonulin.5
Gluten tolerant: The upregulation of zonulin and the opening of the tight junctions is transient, and any leakage of gluten aggregates is appropriately eliminated without the activation of an inflammatory response.
NCGS: The opening of the tight junctions may be less transient, and the leakage of gluten aggregates initiates a continuous inflammatory response rather than simple elimination of the aggregate.
CD: The opening of the tight junctions by is longer and to a higher degree than in the tolerant and NCGS people. This might be why people with celiac disease have a higher chance of developing other autoimmune conditions.
Regardless of the severity of the effect of upregulated zonulin, any degree of intestinal permeability should be avoided if possible, considering the connection between intestinal permeability and the development of autoimmune diseases.

4. Gliadin Can Also Cause Inflammation
Wheat gliadin can directly contribute to inflammation in an immune system that’s already compromised by leaky gut. Sayer Ji, founder of GreenMedInfo.com, references a study in his article “The Dark Side of Wheat” that sheds light on the fact that wheat gliadin can trigger an inflammatory response, even in people who don’t make antibodies to the gliadin directly.
Ji uses a study published in GUT in 2007 to demonstrate this point. The authors of this study conclude that in all individuals tested, there was an activation of the interleukin-15 (IL-15) mediated inflammatory pathway in response to exposure to gliadin peptides in the intestines.
The authors reveal that the difference between CD and non-CD individuals is that the IL-15 mediated response elicits an adaptive response in CD patients that’s absent in non-CD individuals. However, Ji emphasizes the fact that it’s unknown how or when the adaptive response may be initiated, leading to gluten sensitivity or full-blown CD. Development may be contingent on a combination of genetics, environmental exposures, and other disruptions to a properly functioning immune system.6

5. Consuming Gluten Can Create Addictions
In the book Wheat Belly, Dr. William Davis, MD, describes the many different issues that have developed from the consumption of modern wheat. The book includes a summary of Dr. Christine Zioudrou’s findings from her research with the National Institute of Health, documenting what happens to gluten in a simulated digestive system.
The results showed the formation of specific polypeptides from gluten protein that were able to cross the blood-brain barrier and bind to opiate receptors in the brain. With repeated exposures to these morphine-like substances, termed gluteomorphins, Davis explains that the opiate receptors in the brain can become downregulated, with the need for more stimulation to elicit an equal response.
Thus, repeated dosing with these gluteomorphins can lead to craving more gluten and other addictive foods like sugar and dairy in order to achieve the same gluten high. This can contribute to overeating and binge eating disorders and weight gain.
Furthermore, since we depend on the activity of these opiate receptor sites in the brain to maintain our good mood, the downregulated (decreased activity) receptors can contribute to mood swings, anxiety, and depression.
6. Proteins Within Gluten Can Wreak Havoc
IgA and IgG α-gliadin antibodies are the only antibodies tested and used as markers of CD (and sometimes NCGS). However, these gliadins aren’t the only gluten peptides that are irritating and toxic to the intestines.
There are many different types of gliadin proteins identified to be toxic and inflammatory, and more unidentified types most likely exist but haven’t been identified yet.7,8
In a study from 2011, researchers examined the IgA and IgG response of multiple gluten peptides, including α, γ, and ω-types in patients with CD and Crohn’s disease.8 The authors comment on the fact that the immune response among subjects is largely individual, with no two cell samples having the exact same immunologic response to the tested antigens.
Interestingly, the authors point out that one of the participants’ T-cell lines used in the assay didn’t produce an immune response to any of the gluten peptides tested.
This study highlights the individuality of immune responses to different gluten proteins, as well as the possible existence of unidentified aggravating gluten peptides or antigens in wheat that contribute to the development of CD.
However, the variety of gluten peptides may also be important to consider for people who are NCGS or seemingly tolerant. Since there are many different peptides and different people react differently to each, it could explain why the symptoms of gluten sensitivity are varied and often misdiagnosed.

7. This Isn’t Your Great-Grandmother’s Wheat
Another factor in immune system sensitivity to gluten is the unnatural evolution of ancient wheat to achieve the wheat we have today.
The wheat gluten that has been linked to so many health issues today isn’t the same wheat gluten that occurs naturally in wild wheat.
Modern wheat has been bred to be high-yield, bug-resistant, and dwarfed, and it now makes up 99% of wheat products worldwide according to a statistic reported by Davis in Wheat Belly.
Additionally, today’s super wheat is almost three times more genetically complex than Einkorn wheat, the original wild wheat strain. Although genetic complexity sounds like an advancement, it isn’t necessarily better if the humans haven’t adapted at a similar rate to deal with it.
Davis gives a thorough overview of the history of wheat evolution in his book, detailing how human intervention in wheat evolution has drastically increased the genetic complexity of wheat and its corresponding gluten proteins. The gluten protein in our wheat is now found in much larger concentrations, demonstrates much greater variety, and exists in altered ratios. These factors may explain why, according to Davis, there has been a fourfold increase in CD in the past 50 years that can’t be attributed to advancements in diagnostics alone.
8. Science Hasn’t Figured Out Why Tolerance Can Turn into Intolerance
“But I don’t have CD or NCGS,” you might say. A consideration for removing gluten from your diet might be that what mediates the transition from gluten tolerance to CD or NCGS isn’t understood.
Genetics: Although particular genes like HLA-DQ2/8 have been associated with both NCGS and CD, it isn’t necessary to carry these genes to develop celiac disease. It’s likely that there are multiple genes involved in the development of gluten-related disorders.9 You’re also at an increased risk if you have family member with autoimmune conditions.
Epigenetics: The expression of your genes is heavily dependent on the exposome, or the collection of external factors a person may be exposed to in the course of their life. This would explain the variances in the time of onset of CD and NCGS symptoms between genetically predisposed people.10 It has been shown that gut dysbiosis, birth by C-section, and lack of breastfeeding are related to the pathogenesis of CD.
Development of CD and NCGS may also be affected by physical or emotional trauma, stress, infection, and exposure to toxins such as heavy metals, organic solvents, air pollution, toxic mold, or dietary toxins. All of these factors have a cumulative effect over time, so the more you’re exposed to them, the greater your chances are to develop NCGS or CD.

Reason #9: CD and NCGS Can Contribute to Other Chronic Diseases
Since we can’t predict with certainty that we will NOT develop a gluten-related disorder, especially when diagnoses are increasing at an alarming rate, it’s important to understand the risks of developing an immune response to gluten.
Chris Kresser emphasizes the many diseases and symptoms associated with CD and NCGS in his book The Paleo Cure. The following lists are taken directly from Kresser’s work:
Diseases associated with CD: Type 1 diabetes, multiple sclerosis, dermatitis herpetiformis, autoimmune thyroid disease, osteoporosis, heart failure, depression, ADHD, arthritis, migraines, allergies, asthma, and obesity.
Symptoms associated with NCGS: IBS-like symptoms (abdominal pain, bloating, changes in stool frequency), difficulty concentrating and memory issues, headache, fatigue, joint and muscle pain, numbness and tingling in the arms and legs, dermatitis (rash), depression, and anemia.
David Perlmutter, MD, is a neurologist and author of the book Grain Brain, in which he documents the damaging effects of wheat on the brain in particular. Perlmutter identifies NCGS more specifically as a neurological disorder in which gliadin antibodies can actually cause brain damage, dementia, and contribute to the development of Alzheimer’s disease.
So as you can see, regardless of where you fall on the gluten sensitivity spectrum, there are many reasons why you ought to avoid gluten altogether. In the interest of variables ranging from vanity (weight loss, clearer skin, etc.) to great health (digestive ease, pain reduction, looser joints, etc.), give the gluten a rest and see how you feel.
