What Your Yellowish Skin Tone is Telling You
In the third and final installment of the Back To The Future trilogy, Buford “Mad Dog” Tannen asks Marty McFly if he’s “yellow.” As fans of the cult flick will recall, Marty turns around and exclaims: “Nobody calls me yellow!”
While the implication of cowardice is absent for those who are literally yellow, the defensive reaction isn’t far off. Nobody likes to be looked at as though they have a third eyeball, and depending on the severity of the hue, a yellowish appearance to the skin can look very odd to some.
The first (and most common) indication of Jaundice is yellow pigmentation of the skin, eyes, and mucous membranes of the mouth as a result of bilirubin accumulation in the blood.
Jaundice itself isn’t a disease, but rather an indication of underlying health issues that range from the mundane to the severe. Let’s dive into the details of what jaundice is all about, as well as the root causes behind it.

What Exactly is Jaundice?
As previously mentioned, Jaundice is characterized by a yellowish pigmentation of the skin, eyes and mucous membranes in the mouth.
Jaundice isn’t an illness, but a medical condition caused by excessive amounts of bilirubin in the blood stream.
Bilirubin is a brownish yellow substance produced when the liver breaks down old/defective red blood cells as part of the red blood cells natural life-cycle.
Bilirubin is typically removed from the body through stool and is what gives feces its brownish color. Jaundice is most common among newborn babies and typically lasts a few days to one week. However, Jaundice in adults can be indicative of deeper underlying health issues, the causes of which should be investigated swiftly.

How does Jaundice Occur?
Jaundice occurs due to the body’s inability to process bilirubin, the causes of which can stem from :
Excessive red blood cell destruction: Bilirubin is the by-product of hemolysis (the breakdown of red blood cells). If the rate of red blood cell destruction dramatically increases, the liver will be unable to excrete it fast enough.
Dysfunctional bilirubin metabolism: Bilirubin is metabolized in the liver as a result of regular hemolysis. However, if liver cells are injured, inflamed, or unable to function properly, the liver will not be able to remove bilirubin, causing accumulation in the blood.
Obstruction: The normal process of bilirubin metabolism involves excreting bilirubin from the liver in the form of bile, (a liquid released into the digestive tract that aids with the digestion of lipids). A physical obstruction that prevents bile from leaving the liver can also cause bilirubin accumulation.
Immature liver: The most common cause of “Infant Jaundice” that afflicts newborns as a result of their liver’s inability to process bilirubin. Infant jaundice tends to be mild, doesn’t require invasive care, and typically resolves itself within 1-2 weeks.10

Types of Jaundice
Jaundice is typically categorized by which stage of bilirubin metabolism is disrupted, such as:
Pre-hepatic: Jaundice that is caused by a dramatic increase in the rate of red blood cell destruction. Examples include malaria, sickle cell anemia, and kidney disease.11
Hepatic: The inability of liver cells to metabolize and excrete bilirubin, usually as a result of cellular-liver damage from hepatitis, cirrhosis, or alcoholic liver disease.11
Post-Hepatic: Also known as obstructive Jaundice, occurs when the liver is unable to drain bile due to an obstruction. Common causes include gallstones, pancreatic cancer, and parasites.11
Neonatal: Jaundice caused by an infant’s inability to excrete bilirubin from the blood as a result of an immature liver. As previously mentioned, Neonatal Jaundice is usually harmless and lasts for only a few days.11

Root Causes of Jaundice
The root causes of jaundice can be single or multiple in origin.
Premature birth: Infants born prematurely are more likely to develop Jaundice due to an underdeveloped liver. However, bilirubin blood levels typically decrease after 1-2 weeks with no medical intervention necessary.
Reduced blood flow to the liver: Due to severe blood loss from an accident or major surgery, lack of blood to the liver can prevent bilirubin metabolism and excretion.
Impaired liver function: The liver may become overburdened, resulting in slower metabolism and breakdown due to chronic illness, GI infections, certain medications, and exposure to environmental toxins; all of which may trigger jaundice.

Liver disease: Liver cancer, cirrhosis, alcoholic liver disease, non-alcoholic fatty liver disease, and hepatitis all produce liver dysfunction, as well as the inability to absorb/excrete bilirubin.
Bile obstructions: Cholestasis, gallstones, pancreatic cancer, parasites, and pancreatitis create blockages that prevent the drainage of bile from the liver.
Blood cell disease or illness: Malaria, Sickle-cell anemia, and spherocytosis increase the rate at which red blood cells are destroyed, leading to bilirubin accumulation in the blood.
Genetic disorders: Gilbert’s Syndrome, Criglar-Najjar Syndrome, Dubin-Johnson Syndrome, Rotor Syndrome, and Glycogen-Storage disease are associated with jaundice.
Medications and supplements: Certain medications are prone to stressing the liver and causing jaundice.

Root Cause of Jaundice: Liver Disease
Jaundice due to liver disease may occur as a result of:
Liver Cancer (cancer that begins in the liver) is usually caused by chronic infections such as hepatitis, excessive alcohol consumption, diabetes, drug use, and aflatoxins (toxins produced by mold that grows on poorly stored crops and can cause genetic mutations).
The liver is the detoxification organ of the body and filters the blood coming from the digestive tract. This includes metabolizing any drugs or toxins which, in excess amounts, can damage the liver and increase the likelihood of cell mutations.13
When the liver experiences multiple infections, chronic alcoholism, or fatty liver disease caused by diet, obesity, and diabetes, scar tissue begins to build up in the liver tissue, causing cirrhosis. This buildup of scar tissue prevents the liver from properly metabolizing bilirubin.14,16

Chronic alcohol consumption can lead to alcoholic liver disease, one of the most common forms of liver disease in the western world.
Alcoholic liver disease encompasses fatty liver, inflammation, hepatitis, and cirrhosis as a result of excessive alcohol consumption.
Risk factors include the consumption of alcohol without food, one’s gender (women are twice as susceptible to alcoholic liver disease as men), vitamin A and E deficiency, and having a genetic predisposition to either alcoholism or alcoholic liver disease.15,16
Liver inflammation, also known as hepatitis, is typically caused by a viral infection; but as mentioned previously, can also be caused by substance abuse and infection.
Viral hepatitis can be contracted through exposure to contaminated body fluids, foods, or fecal matter. Symptoms are often flu-like, including muscle/joint aches, nausea, headaches, diarrhea, and vomiting.4
Weil’s disease is a severe bacterial infection also known as leptospirosis and is transmitted via animal urine (typically rats, mice and moles). Surfers and white-water rafters are particularly at risk of leptospirosis, which in severe cases can lead to liver damage and internal bleeding.5 Milder symptoms include chills, headache, muscle ache, and conjunctivitis.
Root Cause of Jaundice: Bile Obstruction
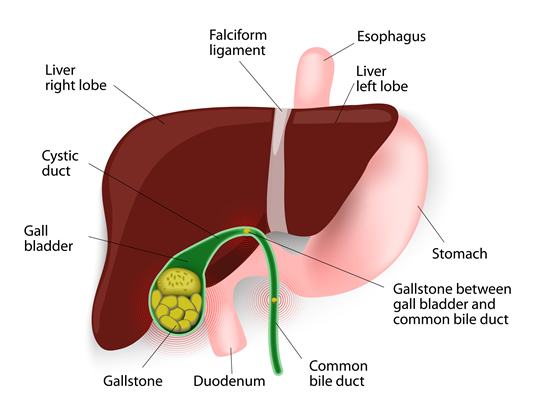
Cholestasis, the medical term for bile obstruction, occurs when bile cannot properly flow from the liver to the small intestine, and is usually the result of:
Gallstone formation in the gallbladder as a result of solid material (stones) comprised of hardened cholesterol or bilirubin particles, that block bile drainage from the liver.
The gallbladder is responsible for storing bile and secreting it into the small intestine during digestion. Gallstones occur in individuals with high cholesterol levels, or those who are genetically predisposed to producing them.
Those who suffer from obesity, diabetes, cardiovascular disease, or other metabolic diseases characterized by high cholesterol levels, are more likely to produce gallstones.
There are certain parasites that gravitate toward the liver, bile duct and gallbladder, which can also impair bilirubin metabolism. Liver flukes and Giardia lamblia are the most common.
Liver flukes exist predominantly where livestock are reared and infect those who swallow the parasite directly. This typically occurs through consuming contaminated food or drinking water.6
Giardia infection also results from ingesting contaminated food, water, or by swimming in contaminated rivers or lakes.
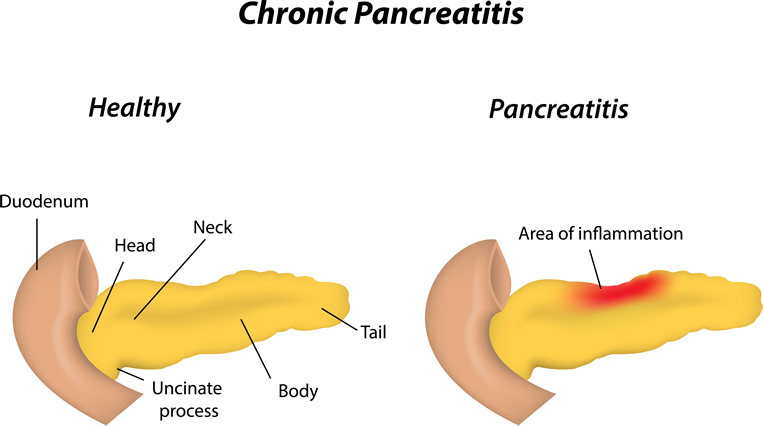
The pancreas is responsible for releasing bile and digestive enzymes into the small intestine during digestion. It’s also responsible for producing the hormones insulin and glucagon to manage blood glucose levels.
Diseases of the pancreas, such as pancreatitis and pancreatic cancer, can prevent bile from getting into the small intestine for excretion.
Pancreatitis (inflammation of the pancreas) is typically the result of gallstones, infections, heavy alcohol use, high blood triglyceride levels, or metabolic syndrome.
Pancreatic cancer can result from smoking, obesity, diabetes, infection, and certain genetic disorders. Symptoms of both pancreatitis and pancreatic cancer include loss of appetite, fever, upper abdominal or back pain, nausea, vomiting, and blood clots.

Root Cause of Jaundice: Blood Cell Diseases
Blood cell diseases that produce jaundice typically occur as a result of increased red blood cell destruction, which the liver is unable to metabolize fast enough. The diseases most commonly responsible for this include:
Malaria, an infectious disease caused by parasites of the genus Plasmodium, is transmitted through the bite of infected Anopheles mosquitoes. Once bitten, the parasite goes straight to the liver.
Sickle-cell anemia, a genetically inherited disease characterized by abnormal hemoglobin (a protein structure in red blood cells that carries oxygen) is the result of abnormally rigid, sickle shaped red blood cells (RBCs) that breakdown rapidly. The irregularly shaped cells can also cause blockages in the liver, compromising bilirubin excretion.
Spherocytosis, similar to sickle-cell anemia, is another genetic condition where red blood cells are misshapen, causing the spleen to mistake them for damaged RBCs and increase the rate at which they’re destroyed.

Root Cause of Jaundice: Genetic Disorders
Symptoms from inherited genetic disorders that cause jaundice are often times mild enough that they go unnoticed.
Gilbert’s Syndrome is a mild genetic disorder that reduces the activity of glucuronyltransferase, an enzyme vital to the metabolism of bilirubin.
Those with Gilbert’s syndrome are more-likely to trigger jaundice through increased stress, dehydration, low calorie diets/fasting, strenuous exercise, and lack of sleep. Other genetic disorders that similarly affect bilirubin metabolism (but are less frequently diagnosed) are Criglar-Najjar syndrome, Dubin-Johnson syndrome, and Rotor syndrome.
Glycogen storage disease is an inherited disease of many subtypes, in which defective enzyme activity negatively impacts glycogen synthesis.
When we consume carbohydrates our body breaks them down into glucose and converts them to glycogen, which is stored in the liver and skeletal muscles for energy production.
Glycogen storage disease causes excessive glycogen buildup, as the defective enzymes can’t break it down properly, leading to liver dysfunction and bilirubin accumulation in the blood.
Natural Relief from Jaundice
Natural management depends on identifying the underlying cause and applying the appropriate treatment. Natural interventions focus predominantly on improving liver health and limiting exposure to toxins, such as:
Avoiding alcohol: Alcohol is processed by the liver and the resulting detoxification reactions cause oxidative stress and can damage liver cells.
Limit toxin exposure as much as possible: Similar to alcohol, toxins such as heavy metals, food additives, food and personal care product preservatives, pesticides, cleaning products, and even medications can be toxic to your liver; depending upon your genetics, exposure, and state of health. Limiting interaction with these substances will reduce oxidative stress and inflammation to the liver.

Consume foods rich in folic acid, vitamin B12, and iron: Adequate folic acid, B12, and iron levels reduce the likelihood of anemia, which can result in nutrient deficiency, and subsequently jaundice.
Consume foods high in antioxidants: Eating a wide array of fruits and vegetables will help decrease inflammation and oxidative stress on the liver.
Liver supporting herbs and nutrients: According to Deepak Chopra, guduchi, an adaptogen that improves the body’s response to stress, anxiety and illness, helps protect the liver from exposure to toxins and reduces liver inflammation.3
Dr. Mark Hyman, M.D. recommends the herbs milk thistle and dandelion, as well as the nutrients lipoic acid and n-acetyl cysteine to support proper liver function.16
