Could Celiac Disease Could Be Sabotaging Your Health?

Could it be that some of your favorite foods are writing your obituary and you don’t even know it?
Have you ever eaten a bagel, pizza, pasta, or bread, or even something that you might not necessarily associate with grains, and then experienced a gut, skin, or mood reaction?
Symptoms can include but are not limited to: a bloated stomach, gas, diarrhea, rashes, irritability, and brain fog. And there are many people who, knowingly or unknowingly, have a mild to severe degree of gluten sensitivity.
Besides the physical manifestations, food allergies and sensitivities can pose real challenges in navigating our daily nourishment. Some of life’s most delicious pleasures, like going out to eat or being invited for dinner, can now be problematic.
The good news is that there’s a burgeoning gluten-free industry, and food options are abundant. In the words of Shauna James Ahern, author and blogger, “After I was diagnosed with Celiac disease, I said yes to food, with great enthusiasm…. I vowed to taste everything I could eat, rather than focusing on what I could not.”
In order to get to the bottom of whether this is a problem for you, let’s look at what exactly Celiac disease is, how it occurs, what the symptoms and root causes are, and natural relief options so that you can get on track toward feeling great.

What Exactly is Celiac Disease?
The USDA food pyramid tells you to have six to eleven servings of grains per day. So you think, surely a nice piece of dark rye bread or those ancient grains like kamut or spelt are good for you. In many cases however, this couldn’t be further from the truth.
Gluten is the protein fraction of most cereal grains, including wheat, rye, and barley.1 Lurking inside some of our favorite foods is this protein that, in the words of Dr. Alessio Fasano, is not digestible by any human kind.2
Celiac disease is regarded as an autoimmune disorder that’s common in the general population with possible onset at any age and with many possible presentations. Gluten is the culprit, and sensitivity to it causes systemic illness that can manifest in a range of organ systems.3
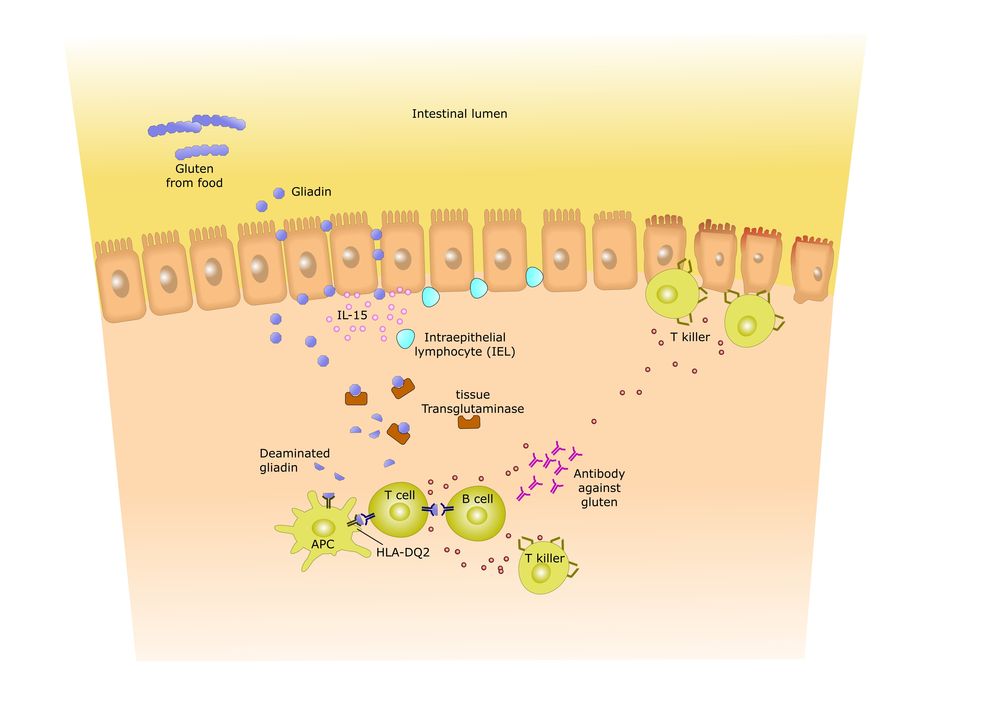
It’s the result of an unchecked immune reaction to gluten. This causes inflammation of the small intestine, where partially-digested gluten proteins contact the gut immune system. This immune response extends beyond just a direct response to the exogenous substance, including a potent and multifaceted immune response to autoantigens (self-antigens) resulting in substantial collateral damage to the structure and function of the gut and other organs.4
Celiac disease is one of the most common lifelong disorders, both in Europe and the US.5 At one time it was considered to be primarily a disease of the intestine, but now we know it can affect the skin, joints, brain, liver, and heart as well.

How Does Celiac Disease Occur?
Celiac disease can occur at any age, from infancy through adulthood. When it occurs later, it’s known as late-onset Celiac disease.
Celiac disease is estimated to affect one in one hundred people worldwide. We’re seeing a rising trend of lower gluten tolerance in humans. This is because the body’s immune system can handle just so many environmental insults. Dr. Tom O’Bryan said in the Gluten Summit, “We have a limited number of options to an unlimited number of offenses.”
Celiac disease is hereditary. People who have a first degree relative with Celiac have a 1 in 10 risk of developing Celiac disease.
When people have unidentified Celiac disease, every time they eat gluten their immune system forms antibodies to gluten that then attack the intestinal lining.
If you have another autoimmune disease such as a Hashimoto’s, rheumatoid arthritis, type 1 diabetes, or primary biliary cirrhosis, you’re at a much greater risk of getting Celiac disease.
It’s important to note that this does not happen overnight. You don’t suddenly wake up one day and have Celiac disease. Dr. Daniel Leffler of The Celiac Center at Beth Deaconess Medical Center states that it takes six to ten years before a person is properly diagnosed.

Symptoms of Celiac Disease
William Davis, MD, author of Wheat Belly, calls Celiac disease the “Great Imitator,” as it’s often misdiagnosed. According to the University of Chicago Celiac Disease Center, there are approximately 300 symptoms associated with Celiac disease.6
There’s a wide array of digestive symptoms associated with Celiac disease, which include but are not limited to abdominal bloating, pain, gas, diarrhea, pale stools, and weight loss.7
Neurological disorders ranging from headaches to impaired cognitive function, psychiatric manifestations, epilepsy, and loss of balance and coordination may also occur with Celiac disease.
The antibodies produced in Celiac may attack nerve tissue, leading to neuropathy. Fifty percent of Celiac patients have peripheral neuropathy, where damage to the nerve affects nerve function, which may cause altered sensation or impaired movement or organ function, depending on the type of nerve affected.
Low mood, depression, and suicidal tendencies are very real symptoms and are common among people on the gluten sensitivity spectrum. The loss of vital nutrients for proper brain function causes vitamin deficiency syndromes as well.

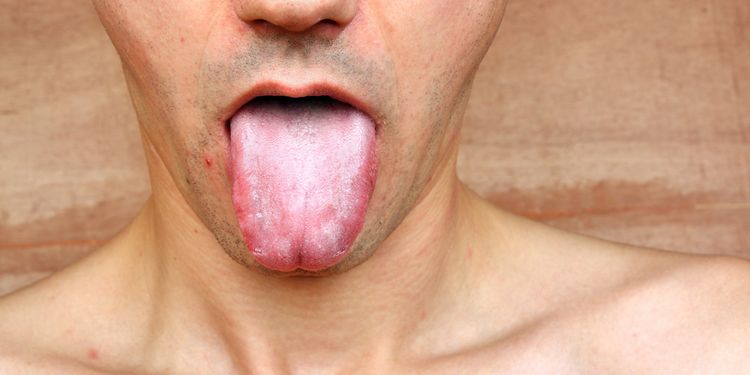
Skin disorders such as skin rash (dermatitis herpetiformis), mouth sores (aphthous ulcers), and discoloration and brittleness of the nails are some of the more common external symptoms.8
Iron deficiency anemia affects 69% of Celiac patients. Deficiencies of vitamin B12, folic acid, zinc, and fat-soluble vitamins A, D, E, and K are also common.9
Dental irregularities such as pitted teeth, grooved, discolored, and poorly-formed teeth can also occur.10 This is most commonly seen as teeth are developing in childhood, but it can appear in late-onset Celiac disease as well.
Failure to thrive is seen in children. This is a big indicator and important marker for parents to be aware of.11 Most babies double their weight by four months and triple it by the time they are one, but kids who fail to thrive usually don’t meet these milestones.
Musculoskeletal problems manifest themselves as muscle cramps or joint and bone pain.
Since we now understand what some of the most common symptoms are, let’s consider the types of gluten sensitivity we may run into.

Variations of Celiac Disease
As with many other chronic conditions, the boundaries of Celiac disease are not always clear. Often referred to as a spectrum, there are currently three known conditions: wheat allergy, Celiac disease, and non-Celiac gluten sensitivity.
With the advent of agriculture, the evolutionary challenge that created the conditions for human disease related to gluten exposure had its roots. Gliadins and glutenins, the proteins found in gluten, are the phytotoxins responsible for wheat allergy and Celiac disease, which are negotiated by the immune system. Its mechanism is T-cell activation in the gastrointestinal mucosa.

In wheat allergy, we see a different response. The cross-linking of immunoglobulin E (IgE) by repeated sequences in gluten peptides triggers chemical mediators such as histamine.
Celiac disease is an autoimmune disorder, where the body mounts an attack against itself through specific autoantibodies.12
Think of it as a branch of the armed forces. Let’s say IgE is the Army, it goes after the enemy, histamine, but instead starts attacking itself in confusion. That’s precisely what’s going on in an autoimmune reaction.
Wheat allergy is an adverse immunologic reaction to wheat proteins. The manifestations are a classic food allergy affecting the skin, gastrointestinal or respiratory tracts, occupational asthma (baker’s asthma), and inflammation of the mucous membrane of the nose (rhinitis).

Celiac disease is an immune-mediated disease triggered by the ingestion of gluten by susceptible individuals. The onset of symptoms is usually gradual, and for every symptomatic individual, there will be eight with no (gastrointestinal) symptoms.
This is where we see the chameleon effect of Celiac disease, as the symptoms vary tremendously from person to person and appear to depend largely on the length and severity of small intestinal damage.
The majority of Celiac patients have visited five or more doctors prior to diagnosis—and it can take an average of eleven years after initial presentation for Celiac disease to be diagnosed.13
Celiac disease is the result of an unchecked immune reaction to gluten. The mechanism goes way beyond a reaction to an exogenous substance—it includes a potent and multifaceted response to autoantigens (self antigens), resulting in substantial collateral damage to the structure and function of the gut and other organs.14 Increased intestinal permeability (leaky gut) is an early biological change that precedes Celiac disease.
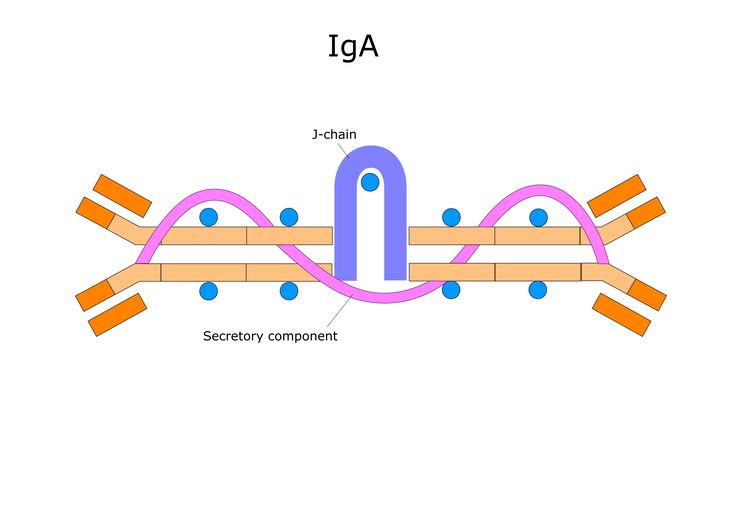
 Non-Celiac gluten sensitivity is a condition where laboratory results are negative for IgA against transglutaminase (TTG) and positive for IgG or IgA against gliadin.
Non-Celiac gluten sensitivity is a condition where laboratory results are negative for IgA against transglutaminase (TTG) and positive for IgG or IgA against gliadin.
In non-Celiac gluten sensitivity, symptoms are triggered by gluten ingestion with the absence of a disease of the small intestine, which is how it differs from Celiac.
The immune system mounts a response but does not destroy the lining of the intestines as it does with the autoantibodies (antibodies against your own tissues) created in Celiac.
Exposure to gluten as small as one eighth of a thumbnail, or 20 PPM (parts per million), is enough to cause an immune response. It’s also not dose-dependent, meaning that if you have one bite or the whole piece of bread, the immune response generated will be the same.

The most common complaints are brain fog, bloating, diarrhea, fatigue, and numbness in legs, arms, and fingers. Several studies are suggesting a relationship between non-Celiac gluten sensitivity and neuropsychiatric disorders, particularly autism and schizophrenia.
We see the chameleon-like nature of gluten sensitivities as there’s an overlap between irritable bowel syndrome (IBS) and gluten sensitivity, and with the lack of biomarkers, diagnosis is difficult.15,16
Dr. Hyman states, “An estimated 99% of people who have a problem with eating gluten don’t even know it. They ascribe their ill health or symptoms to something else—not gluten sensitivity, which is 100% curable.”

Root Causes of Celiac Disease
Celiac disease has many potential root causes that are directly related to the presence of gluten, combined with genetics and lifestyle factors.
Exposure to gluten before three months of age.19 There’s a five-fold increased risk in infants fed wheat, barley, or rye cereals prior to three months of age.
Breastfeeding status is important. Non-breastfed babies have a higher risk of developing Celiac disease.20 Because of the immuno-protective properties in colostrum and mother’s milk, the likelihood of developing Celiac disease is much higher in those babies not breastfed.
Genetics play a role in developing Celiac, as certain people have a genetic predisposition.21 The gene is HLA, and there are two forms called DQ2 and DQ8. In the words of Dr. Fasano, “All Celiacs with very, very rare exception will have either one or both.”
Major life events can be a trigger, such as emotional stress, pregnancy, and surgery.22
Faulty immune function may cause your immune system to mistakenly attack its own tissues triggered by eating gluten in food.
Antibodies from the gluten exposure attack the intestinal lining, damaging, flattening, and destroying the microvilli—tiny hair-like projections that cover the small intestine.2
Having one autoimmune disease increases the risk of getting another, including Celiac disease.21 When your immune system attacks your body in one way (as with Hashimoto’s or Type 1 Diabetes), there’s a good chance it will attack other tissues too.
Autoimmune diseases tend to co-mingle. Dr. Gerald Mullin, MD and functional gastroenterologist has stated, “Statistically, someone with an autoimmune disease is at risk, if they don’t put the fire out, of having a total of seven autoimmune diseases in their life.”

Candida albicans may stimulate the formation of antibodies to gluten.24 There’s a mirror-like effect that can occur between these two conditions where the presence of either one can stimulate the other condition.
Exposure to hybridized wheat and pesticides such as glyphosate is one of the most important factors to understand.
Modern American wheat is hybridized using traditional methods (not GMO) that increase the amount of gluten, which increases your chances of reacting to it. Glyphosate, found in the herbicide Roundup®, is used in the end stage of wheat harvesting and is implicated in causing collateral damage to the gut.
Gluten cross-reactive foods can be significant triggers, especially in people that have not responded well to the removal of gluten in their diet. These foods are molecularly similar to gluten, and the body responds to them in the same manner.

Root Cause of Celiac Disease: Early Exposure to Gluten
Exposure to gluten before three months of age in high-risk children increases the likelihood of developing Celiac disease.19
Several studies over the years have characterized this risk, with results showing children exposed to gluten before 3 months of age can be up to five times more likely to develop Celiac disease than those with gluten introduced after they get a little older.
At this point in development, the gut of an infant is still too immature to handle the gluten proteins and may develop a sensitivity or Celiac as a byproduct of repeated early exposure.
What’s somewhat unexpected is that the same studies also spotted an upper age limit, after which the risk of developing Celiac disease starts to increase again. Early results showed that if children were not exposed to gluten until after they’re 7 months old, they had a twofold increased risk compared to those who started receiving gluten before.19
Root Cause of Celiac Disease: Lack of Breastfeeding
Breastfeeding status can have a profound effect on whether or not a child will get Celiac disease.
Due to the immuno-protective properties in colostrum and mother’s milk, the likelihood of developing Celiac disease is much higher in those babies not breastfed.20
The immune system is one of the human body’s most unique and least understood functions.
Innate immune capability is limited at birth, and the baby is relying heavily on Mom for immunity. However, by the end of the first year of life, immune function is fully operational.
During this maturing process, immune protection is provided by maternal antibodies transferred from mother to infant prior to birth. An additional mode of maternal immune support can be provided via breast milk feedings. Human breast milk contains numerous protective immune components, including secretory immunoglobulin A (sIgA) antibodies.
Some researchers suggest that sIgA antibodies are important in reducing or delaying onset of clinical symptoms in infants at risk for Celiac disease.

In 2002 Ivarsson et al. were able to show that risk of CD was reduced in children less than two years of age if they were being breastfed at the time dietary gluten was introduced.
The risk was also reduced if the amount of gluten introduced was a small or medium amount. Additionally, the protective effect of breastfeeding was pronounced if breastfeeding was continued after introduction of dietary gluten.
These researchers concluded that gradual introduction of gluten-containing foods while infants are still being breastfed is beneficial in reducing risk of CD, and this benefit may extend into early childhood.20
Root Cause of Celiac Disease: Genetics
Genetics plays one of the biggest roles in who will get Celiac disease and who won’t.21
The risk of developing CD is increased by certain variants of the HLA DQ2 and HLA DQ8 genes.
These genes provide instructions for making proteins that play a critical role in the immune system. The HLA gene complex helps the immune system distinguish the body’s own proteins from proteins made by foreign invaders, such as viruses and bacteria.
This complex, which is present on the surface of certain immune system cells, attaches to protein fragments outside the cell. If the immune system recognizes the peptides as foreign, it triggers a response to attack the invading viruses or bacteria.
Celiac disease is associated with an inappropriate immune response to a segment of the gluten protein called gliadin. This inappropriate activation of the immune system causes inflammation that damages the body’s organs and tissues and leads to the signs and symptoms of Celiac disease.21

Root Cause of Celiac Disease: Major Life Events
Major life events are important when considering the potential development of Celiac disease.22
A major life event can be anything that causes significant stress, such as the birth of a child, marriage, divorce, job loss or gain, relocation, surgery, or illness.
Stress can play a significant role in the evolution of many chronic diseases, especially those that are gut-related, as stress mediates chemical changes that actually decrease immune system function, as well as the antibody secretory IgA (sIgA), which is the gut’s first line of defense.
Additionally, stressful life situations often cause people to seek medical advice, as pre-existing symptoms suddenly appear very important in their current moment of stress.
An article from the American Journal of Gastroenterology August of 2012 on the incidence and risk of CD in a healthy US population showed a five-fold increase among active servicemen. Prior to deployment in Operation Iraqi Freedom, there was a lower risk of Celiac disease; however, following active duty, there was an increased risk of gastrointestinal disorders that manifested in the third, fourth, and fifth decades of life. This was attributed to the great deal of stress endured during deployment.

In another study published in Nutrients, September 2013, the outcome revealed it was the number of stressful life events in the Celiac disease group and not their severity necessarily that initiated the onset of the immune-mediated disease. Ongoing stress can be just as harmful as one or two major stressors.
The main takeaway here is that stress in any form alters the immune system and gut function, and it perpetuates inflammation, which all increase the chance of developing CD.
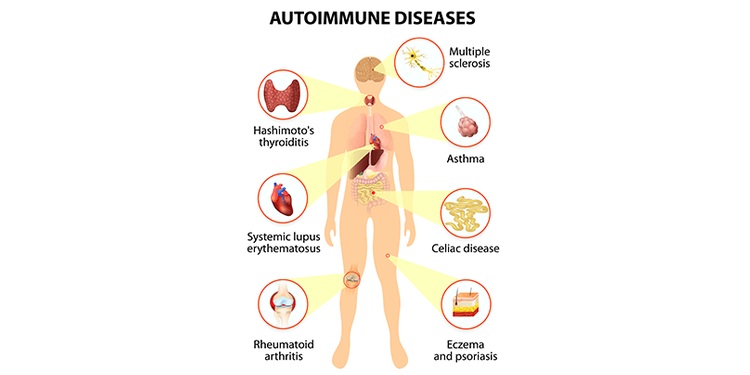
Root Cause of Celiac Disease: Autoimmune Disease
Autoimmune disease: Having any of these other autoimmune diseases immediately places you at higher risk for developing Celiac disease:
- Type 1 Diabetes
- Hashimoto’s thyroiditis
- Graves’ disease
- Ulcerative colitis
- Microscopic colitis (lymphocytic or collagenous colitis)
- Lupus
- Crohn’s disease
- Vitiligo
- Down’s syndrome or Turner syndrome
- Addison’s disease
- Sjogren’s disease
- Pernicious anemia
- Scleroderma
- Chronic autoimmune hepatitis
- Dermatitis herpetiformis
- Polymyalgia rheumatica
- Auto-antibody hemolytic anemia

The way your body develops Celiac or additional autoimmune (AI) conditions when you already have one is the same for all AI diseases.
Normally, the immune system has the ability to distinguish between self and non-self—what’s you, and what’s an invader.
When you have an AI condition, the body is already programmed to attack itself, and sometimes the presence of a bacteria, virus, parasite, or a food antigen (such as gluten) can stimulate an immune attack on additional “self” tissues.
During a quick, mounted immune response, the body sometimes begins making antibodies and attacking normal cells by mistake in response to the “invader.” At the same time, special cells called regulatory T-cells fail to do their job by keeping the immune system in line, further complicating the situation.
Root Cause of Celiac Disease: Candida Albicans
Candida albicans is a type of yeast that can trigger the onset of Celiac disease. Having a Candida infection may stimulate the formation of antibodies to gluten as well as autoimmune antibodies that are found in many people that have CD.24
Recurring yeast infections can increase gliadin IgG antibodies in your body, which are the same antibodies that your body makes when you have Celiac disease.
The same mechanism of disease found in Candida albicans is present in Celiac disease. The internal environment where the pathogens are able to find their niche and colonize is the same in both diseases.
The identical sequence of proteins that’s found in CD occurs in the cell walls of Candida. These Candida gluten-like proteins turn out to be yeast’s “velcro,” allowing them to attach and hang on to the tissue transglutaminase and endomysium in the wall of the intestine.
In Celiac disease, the antibodies produced attack these same structures, which destroys the intestinal lining.
Since Candida can trigger the same chemical and immunological reactions as found in Celiac disease, CD can also trigger Candida infection. If you have Celiac disease, symptoms usually get better rapidly with the elimination of gluten from your diet. However, this isn’t always the case. This may be an indication of intestinal Candidiasis

Root Cause of Celiac Disease: Hybridized Wheat
Modern American wheat is very different from the ancient grain it’s derived from.
Agricultural advances have allowed scientists to hybridize the wheat by crossing different wheat strains to improve characteristics, such as to produce more gluten.
They are then backcrossed, hybridized with non-wheat plants, and possibly exposed to mutagens such as radiation or chemicals to produce optimal characteristics. This is what modern, gluten-heavy American wheat is today.
“It’s not a GMO, but can be worse,” according to Dr. William Davis.27 This high-gluten, altered wheat is foreign to the immune system, and it reacts accordingly, resulting in gluten sensitivity and Celiac disease.

The active ingredient used as an herbicide in wheat harvesting is glyphosate. According to Dr. Stephanie Seneff, the use of glyphosate on wheat crops has risen in tandem with the rise in Celiac disease.25
She says that the presence of glyphosate in Roundup® “is the most important causal factor in this epidemic.
Celiac disease is associated with imbalances in gut bacteria that can be fully explained by the known effects of glyphosate on gut bacteria.
Characteristics of CD point to impairment in many cytochrome P450 enzymes, which are involved with detoxifying environmental toxins, activating vitamin D3, catabolizing vitamin A, and maintaining bile acid production and sulfate supplies to the gut. Glyphosate is known to inhibit cytochrome P450 enzymes.”
Also, reproductive issues associated with Celiac disease such as infertility, miscarriages, and birth defects can also be explained by glyphosate. Recent animal studies have revealed a disruption in gut bacteria, killing off beneficial forms and causing an overgrowth of pathogens. Many of the features seen in these studies are reminiscent in Celiac disease.

Root Cause of Celiac Disease: Cross-Reactive Foods
You’ve gotten off gluten, are experimenting with some gluten-free recipes, but are still experiencing upset stomach, brain fog, and headaches. It could be that these foods are cross-reactive. This means that they contain the same or a similar amino acid sequence as wheat.
Dr. Perlmutter tells us, “For example, about fifty percent of people that are gluten-intolerant are also sensitive to dairy. Even coffee can be problematic, as it tends to cross-react with gluten and can mimic symptoms of gluten-intolerance.”
Some grains you’ll want to be weary of include buckwheat, sorghum, millet, spelt, amaranth, quinoa, kamut, hemp, yeast (baker’s and brewer’s), tapioca, teff, corn, oats, and rice.
In addition, here are some proteins that can be problematic: whey, eggs, all dairy products, and soy. Other foods to be aware of are chocolate, sesame, eggs, coffee, and potatoes. These food will elicit the same immunological response as gluten and should be avoided.
Similarly, another group of foods known as FODMAPs (Fermentable, Oligo-, Di-, Monosaccharides and Polyols), which are short-chain carbohydrates and sugar alcohols that are difficult to absorb and digest, may also drive symptoms in some individuals.26
FODMAPs include many of the foods listed above along with foods made with high fructose corn syrup, certain fruits, vegetables, and mushrooms.

Natural Relief from Celiac Disease
Healing the gut is of utmost importance in dealing with the spectrum of gluten sensitivity or Celiac.
Your microbiome has a huge impact on your health, especially the ability to synthesize vitamins and nutrients, digest food, and combat inflammation. It’s your first line of defense. Inside your gut microbiome lives hundreds of trillions of bacteria.
Probiotics will aid in repopulating your microbiome with beneficial bacteria. Some very good sources of probiotics are yogurt, kefir, sauerkraut, kimchi, pickles, and other fermented foods.
You can also purchase probiotics in pill form. Most require refrigeration, but some do not. Make sure you purchase a high-quality, multi-species probiotic.
According to Dr. Tom O’Bryan, “There are various bacterial ‘strains’—this concept is similar to the breed of a dog. All dogs are of one species, but a German Shepherd is used differently for specific tasks than a Chihuahua.” Having a multi-species probiotic ensures you’re getting a broad spectrum of bacteria strains.
Digestive enzymes are powerful tools in breaking down gluten proteins. Some enzymes you want to look for are HUT Protease and SAPU-Exo-peptidase.
Colostrum is supportive in healing the gut.
Supplements related to Celiac and gluten sensitivity include vitamin D3, zinc, EPA/DHA, L-Glutamine, curcumin, B vitamins, magnesium, and calcium as these help heal the gut, modulate the immune system, and provide additional nutrients that may be malabsorbed depending upon the state of your gut.

Above all, you want to be following a gluten-free diet. In the consensus of the World Gastroenterology Organization, “The only treatment for Celiac disease is a strictly gluten-free diet for life.
No foods or medications containing gluten from wheat, rye, and barley or their derivatives can be taken, as even small quantities may be harmful.”18 Add to this oats, corn, rice, sorghum, millet, and buckwheat.19
Be very careful about hidden sources of gluten that are not easily detected or known. Who knew beer and soy sauce could be sabotaging our health?
According to Aristo Vojdani, consuming gluten-based foods and alcoholic beverages together greatly intensifies the impact of antigens. Having that beer and pizza together overwhelms the digestive system because it solubilizes a significant amount of gliadin peptides in the pizza.
Finally, be mindful of hidden sources of gluten in personal care products as well, as certain cosmetics and skin care products often contain gluten. Look for products that are specifically labeled gluten-free, and do your homework before you put anything foreign on your body.
